Abstract:
In the province of the Khyber Pakhtunkhwa (K.P.), maternal and neonatal mortality is alarmingly high. To cope with MNCH challenges, cost-effective and low technology intervention like Continuum of Care (CoC) is required. This study examines ANC visits, delivery assisted by SBA, and PNC to determine CoC for maternal health care (MHC) services in K.P. In doing so, the study analysed primary data from 806 reproductive-age women (15-49) who gave birth in the previous two years. The data has been collected from randomly selected five districts of K.P. namely Peshawar, Swabi, Nowshera, Kohat, and Malakand. Personal, family, reproductive, and community factors are categorised as Predisposing, enabling and perceived need factors. First, bivariate analysis was done to see how these factors associated with ANC, SBA, and PNC visits. Multivariate analysis using the Logit and Probit models has been done to assess results consistency. Multivariate study showed that women's age at first birth, total number of children, years of schooling, husband education, place of residence, health service provider, birth interval, and enrolment in conditional cash transfer (CCT) program were significantly associated with CoC from ANC to skilled assisted delivery and PNC. The results indicate lack of CoC among women in the study area.
Key Words:
Continuum of Care, ANC, PNC, Skilled Birth Attendant, Conditional Cash Transfer
Introduction
In order to improve overall health and preserve the lives of women and their babies, adopting the CoC in K.P. could play an instrumental role. One of the main Sustainable development Goals (SDG) is to reduce maternal and child mortality. Towards this end, promoting antenatal, postnatal visits and the proportion of births by trained birth attendants are important. Pakistan has one of South Asia's highest maternal death rates notwithstanding global declines (UNFPA, 2013). It remained at 186 deaths per 100,000 live births in 2019, indicating Pakistan still confronts challenges in decreasing maternal and child mortality and lagging to fulfill its SDG targets. Pakistan's MHC services are underutilised compared to other developing countries. Most maternal and neonatal deaths in K.P. occur after birth and postpartum. Many such fatalities go undetected due to cultural difficulties and humiliation. The report by DHIS (2018) claims maternal deaths of 383 women out of 228936 deliveries of which 167 deaths occurred at government health facilities. Most maternal deaths can be avoided (Bustreo et al., 2013) if MHC services are available and given in a continuous manner, as recommended by the Continuum of Care (CoC) strategy (Bhutta et al., 2014). According to WHO, more than half of women and babies in underdeveloped countries don't receive MHC during and after birth. Despite having community midwives, trained birth attendants, and lady health workers, K.P.'s MNCH utilisation is minimal.
CoC improves maternity, newborn, and child health (MNCH) outcomes by integrating time and place factors (Iqbal et al., 2017; Berhan et al., 2014). Timely care throughout the lifecycle improved maternal and neonatal survival and health whereas, place dimension connects homes, communities, and hospitals. (Kerber et al., 2007; Iqbal et al., 2017; Yeji et al., 2015; Akinyemi et al., 2016). It encourages women to choose a skilled delivery provider, reducing mother and infant death and disability (Campbel et al., 2006; Darmstadt et al., 2005; Rockerset al., 2009)
Most women in K.P. do not seek MHC and almost half do not give birth in a hospital (Bhutta et al. 2013). As a result, most deliveries in K.P. still take place at home (NIPS, 2013). Further, ANC, PNC, and delivery supported by a SBA as well as institutional delivery have been demonstrated to lower maternal and child mortality (Bustreo et al. 2013; WHO 2014a). This study examines ANC, SBA, and PNC from pregnancy to birth to determine CoC's MHC service continuity. It represents the need for optimal care when risk of complication for mother and child is the highest (de Graft et al., 2006).
Conditional cash transfers (CCT), a demand-side program, encourage households or pregnant women to seek MHC services. These financial incentives aimed to promote preventive care thus, improved health outcomes. In places where institutional births are still low, economic incentives are utilised to promote MHC and institutional births. Nepal, India, and Bangladesh all have similar policies. Financial incentives are meant to improve health outcomes by shifting health expenditures and/or consumption patterns. In March 2014, the K.P. government started giving pregnant women Rs. 2700 stipend. K.P. Chief Minister (CM) initiative for MCH encourages pregnant mothers to attend ANC, PNC, and SBA checkups. To successfully apply CoC, underutilised ANC, SBA, and PNC variables must be analysed. Demographic and socioeconomic factors also affect MHC use.
Previous research studies have examined the impact of related factors on MHC usage (Govindasamy and Ramesh, 1997;. Thind et al., 2008; Dixit et al., 2013; Chandrashekar, 1998; Chakaraborty, et al., 2003; Dwivedi, 2009; Baral et al., 2010; Joshi et al. 2014; Karkee et al. 2013; Khanal et al., 2011). These studies mostly focused on one component MNCH service (ANC, SBA, PNC), therefore, missing the CoC. So far, no research has been done in K.P. on factors related to underutilisation of MHC services given the CCT and CoC theory. Thus, this evaluated ANC, SBA, and PNC as an integrated MHC to examine the CoC in K.P. The study used primary data from 806 pregnant females from Peshawar, Swabi, Nowshera, Kohat, and Malakand districts.
Here's how the paper continues. Second portion covers conceptual framework followed by empirical analysis. Section three discusses the study area and data collection, whereas section four explains empirical results and related discussion. The last and final section represents conclusion and policy recommendations.
Conceptual Framework Continuum of Care (CoC) & Three Delay (3D) Model
A functional continuum of care is sensitive to newborn health because it depends on effective links between maternal and child health programs and reducing delays in care for difficulties during and after. Thus, this study connects CoC theory with the "Three Phases of Delay Model" (Andersen, 2005; Thadeus & Maine, 1994; WHO, 2005) because it is used to define factors related with underutilisation of MHC services. As indicated in the figure 1 below, a successful CoC connects vital MNCH services during adolescence, pregnancy, childbirth, postnatal and neonatal periods, and into childhood.

Connecting Care Through Out the Crucial Time Periods in the Lifecycle
Thaddeus and Maine (1994) cited insufficient time-dimension care for increased maternal mortality in developing countries. The 3D model has three features and conditions. Delayed decision to seek care when issues arise; Delayed arrival at an obstetric medical institution; then, Delayed receiving of proper and essential care.
Traditional parameters such as prior health system experience, place of residence, transportation availability, road conditions, and cost of transportation and/or distance to health facility influence the decision to seek medical care. Once in the facility, operational challenges in the health care delivery system further impede effective service. The delay model helps develop preventive interventions and strategies by identifying socio-demographic and cultural factors related to maternal death. Numerous sociocultural and socio demographic factors influence maternal mortality in K.P. The three delays model highlighted three factors impacting MNCH service use and access: These are
Phase 1: Delay in receiving treatment: largely attributable to socio-demographic factors
Phase 2: Delay in seeking care: factors
Relating physical and financial availability
Phase 3: Delay in receiving appropriate medical care: variables associated with the quality of facility-based health care.
Material and Methods Study Area, Data Collection and Sampling Procedure
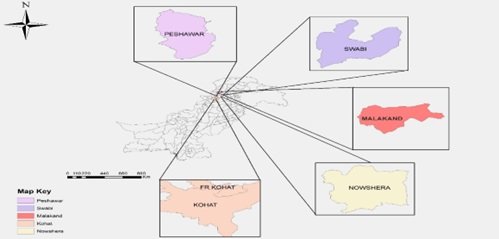
Study districts were Swabi, Peshawar, Nowshera, Kohat, and Malakand (figure 2). Peshawar, Nowshera, and Swabi represent the centre province, Kohat the south, and Malakand the north. These districts' socioeconomic and demographic characteristics make the sample representative. 806 women between 15 and 45 who had birth in the past two years were interviewed using a structured questionnaire. The survey covered socioeconomic, demographic, and reproductive histories from two groups. One that participated in the CCT program (n=408) and a control group (n=398). Beneficiaries and non- beneficiaries were contacted through community midwives (CMW) in a randomly selected union council (U.C.).
Data Analysis
Three CoC-based outcome variables for pregnancy, labor, and postpartum has been constructed. The initial model used ANC as an outcome variable, with a value of "1" for at least one ANC from a trained birth attendant (TBA) and "0" otherwise. The second model focuses on SBA as an outcome and assigns 1 if a woman received ANC and delivery assisted by skilled birth attendant (SBA), 0 otherwise. The final outcome variable is complete CoC as indicated by women who obtained MHC services from skilled physicians. The third model outcome variable is "1" if a woman receives all three types of skilled care and "0" otherwise. To illustrate, the factors that influence MHC services are categorised into the sociocultural, accessibility, and perceived need factors. The study used bivariate and multivariate logistic regression to investigate the connection between these variables and
the outcome.
Independent variables such as socio-demographic characteristics of women (such as age, education, occupation, and her husband's age and education, and occupation), household characteristics (total household size, total household income, family system (Joint/Nuclear), household arrangement (owned/ rented), contextual factor (place of residence, type of house (kacha/pakka) ) maternal and reproductive history ( total number of pregnancies, place of delivery (institution/non-institutional), the complications in previous pregnancies, experience any neonatal mortality or miscarriage (yes/no) are provided in table 1. This study uses information and communication technology (ICT) if the respondent has access to media like T.V., newspapers, radio, listening to the radio, meeting LHV/CMW, or community setting.
Data Analysis
Three CoC-based outcome variables for pregnancy, labor, and postpartum has been constructed. The initial model used ANC as an outcome variable, with a value of "1" for at least one ANC from a trained birth attendant (TBA) and "0" otherwise. The second model focuses on SBA as an outcome and assigns 1 if a woman received ANC and delivery assisted by skilled birth attendant (SBA), 0 otherwise. The final outcome variable is complete CoC as indicated by women who obtained MHC services from skilled physicians. The third model outcome variable is "1" if a woman receives all three types of skilled care and "0" otherwise. To illustrate, the factors that influence MHC services are categorised into the sociocultural, accessibility, and perceived need factors. The study used bivariate and multivariate logistic regression to investigate the connection between these variables and
the outcome.
Independent variables such as socio-demographic characteristics of women (such as age, education, occupation, and her husband's age and education, and occupation), household characteristics (total household size, total household income, family system (Joint/Nuclear), household arrangement (owned/ rented), contextual factor (place of residence, type of house (kacha/pakka) ) maternal and reproductive history ( total number of pregnancies, place of delivery (institution/non-institutional), the complications in previous pregnancies, experience any neonatal mortality or miscarriage (yes/no) are provided in table 1. This study uses information and communication technology (ICT) if the respondent has access to media like T.V., newspapers, radio, listening to the radio, meeting LHV/CMW, or community setting.
Table1. Summary Statistics of the Variable used in the study
|
Variables
|
Units |
Mean |
SD |
|
Age |
Years: continuous |
30.83 |
6.36 |
|
Age at first birth |
Years: continuous |
21.35 |
3.34 |
|
Women total years
of schooling completed |
in years: |
6.26 |
4.15 |
|
Husband's years of
schooling |
in years |
7.85 |
2.77 |
|
Total Household
size |
in numbers |
21.33 |
8.35 |
|
Live pregnancies |
in numbers |
4.53 |
2.014 |
|
Total number of
pregnancies |
in numbers |
5.58 |
2.34 |
|
Health services
provider (Skilled/ Unskilled) |
in numbers |
0.797 |
0.403 |
|
Residence: Rural/
Urban |
Binary Variable |
0
.850 |
0.357 |
|
Exposure to
television |
Binary Variable |
0.641 |
0.48 |
|
Access to the
health facility |
Binary Variable |
0.656 |
0.475 |
|
Birth Interval
(<1/>=2 years) |
Binary Variable |
0.815 |
0.388 |
|
Have you been
vaccinated during ANC |
Binary Variable |
0.757 |
0.429 |
|
TFR Vaccination |
Binary Variable |
0.695 |
0.461 |
Multivariate logistic regression comprised bivariate
correlated variables, as chi-square (X2) has been tested for
categorical data and the F test for continuous variables. Once all independent
variables are incorporated, likelihood probabilities for each model are
calculated to determine the CoC from ANC, SBA, and PNC.
Model Specification
We utilise logistic regression to understand women's propensity to use MHC services offered by a skilled health professional.
Given the logistic function G in the logit model:
p(y=1?x)=G(?_o+?_1 x_1+ ?_2 x_2+?………+ ?_k x_k-------(1)
For all real numbers z, the function G accepts only values between 0 and 1: 0<G_z <1. This guarantees that the predicted response probabilities are always between 0 and 1. For instance, in estimating the logit model, G denotes the logistic function:
G(z)=expz/[1+exp?(z) ] =G(z)-------------------(2)
The probit model cumulative distribution function (cdf) for a standard logistic random variable G is presented below.
G(z)= ? (z)? ?_(-?)^z?? (v)?v-------------------(3)
Where the standard normal density function is ? (z) is specified as:
G(z)= ? (z)=(2?)^(-1/2) exp??(-z^2/2)---------------(4)?
The present study estimates the logit and probit model using the following specification
log?[p_ij/p_i0 ]= ?_0+?_1j X_ij+?_2j Y_ij+?_3j Z_ij+?_ij----------(5)
In this example, the dependent variable is the log chances a lady will choose j over 0 In this scenario, the dependent variable is the log odds that a mother will choose choice j over alternative 0, indicating no SBA in ANC Visits, with ‘1’ suggesting consultation with a physician, nurse, or midwife. Similarly, Models 2 and 3 are estimated in the same way.
Individual-level variables are represented by X, household-level variables by Y, and community-level variables by Z. The model includes a provincial dummy variable. 0 represents fixed effects, while 1, 2, and 3 imply random effects on the CoC from MHC services.
Results CoC Measure of Association with a Number of Fundamental Predisposing, Enabling and Perceived Need Factors
Table 2 shows an association of predisposing factors, i.e. individual women and their household characteristics, along with some enabling and perceived need factors with ANC visits and with SBA. Age is a significant predictor of MHC use. The behaviour model by (Andersen, 1995 & Cropper, 1977) reports that younger generations are more concerned about their health and education compared to older people. Women who had ANC from a trained practitioner are mostly of older age than those who didn't. The variable age was found to be insignificant for the SBA visits. Moreover, the place of delivery and the health service provider (whether skilled or unskilled) also played a significant and positive role in promoting the CoC from MHC services. Access to health facilities was one of the most critical enabling factors related to CoC utilisation. It was discovered that if a respondent had relatively simple access to a health institution, they made more frequent hospital visits. Difficult access to health facilities, on the other hand, deters women from seeking MHC (Khan, Hotchkiss, Berruti & Hutchinson, 2006). ANC use is much higher among respondents with relatively greater access to health facilities than among those who do not.
Table 2
|
ANC |
Care at
Delivery assisted by SBA followed by ANC |
PNC
followed by ANC and Delivery assisted by SBA |
|||||||
|
Variables |
Received |
Did not |
|
Received |
Did not |
|
Received |
Did not |
|
|
Predisposing factors |
Care |
Received
care |
|
Care |
Received
care |
|
Care |
Received
care |
|
|
Continuous Covariates |
Mean
(SD) |
Mean
(SD) |
F-Stat(p
value ) |
Mean
(SD) |
Mean
(SD) |
F-Stat(p
value ) |
Mean
(SD) |
Mean
(SD) |
F-Stat(p
value ) |
|
Respondent age |
30.85
(6.4) |
30.5
(6.3) |
0.15 |
30.872
(6.386) |
29.8
(5.749) |
0.95 |
30.870
(6.377) |
29.621
(5.858) |
1.08 |
|
Respondent age at first birth |
21.46
(3.36) |
20.13
(2.73) |
9.33** |
21.402 (3.331) |
20.286
(3.339) |
3.76 ** |
21.389
(3.323) |
20.414
(3.621) |
2.39 |
|
Respondents total years of
schooling |
6.301 (4.194) |
5.79 (3.655) |
0.87 |
6.249
(4.167) |
6.543
(3.906) |
0.17
(0.6826) |
6.277
(4.172) |
5.862
(3.681) |
0.28 |
|
Husband Age |
36.28 (6.24) |
35.51 (5.71) |
0.91 |
36.309
(6.233) |
34.314
(5.166) |
3.47
(0.0627) |
36.284
(6.225) |
34.552 ( 5.336) |
2.19 |
|
Husband total years of
schooling |
7.899
(2.78) |
7.32
(2.589) |
2.56* |
7.852
(2.781) |
7.886
(2.564) |
0.00
(0.9441) |
7.847
(2.781) |
8.034
(2.514) |
0.13 |
|
Total household size |
21.094 (8.38) |
24.079
(7.57) |
7.48** |
21.223
(8.337) |
23.629
(8.468) |
2.78* |
21.254
(8.331) |
23.310
(8.8) |
1.7 |
|
Number of children |
4.50 (2.039) |
4.86
(1.68) |
1.82 |
4.510
(2.032) |
4.943
(1.533) |
1.55
(0.2137) |
4.508
(2.028) |
5.069
(1.534) |
2.17 |
|
Total number of pregnancies |
5.56
(2.37) |
5.75
(1.9) |
0.32 |
5.584
(2.361) |
5.6
(1.958) |
0.00
(0.9679) |
5.577
(2.358) |
5.793
(1.953) |
0.24 |
|
Categorical Covariates |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
|
Type of delivery (Normal/ C-section) |
698
(86.6) |
108
(13.4) |
0.03 |
698
(86.6) |
108
(13.40) |
0.74
(0.3913) |
698
(86.60) |
108
(13.40) |
1.1 |
|
Place of delivery (Public/ Private) |
653
(81.02) |
153 (19) |
54.39*** |
653
(81.02) |
153 (18.98) |
145.34
(0.00) |
653
(81.02) |
153
(18.98) |
117.69*** |
|
Health services provider
(Skilled/ Unskilled) |
642
(79.65) |
164
(20.35) |
52.27*** |
642(79.65) |
164
(20.35) |
143.23
(0.00) |
642
(79.65) |
164
(20.35) |
117.76*** |
|
Enabling factors |
|
|
|
|
|
|
|
|
|
|
Continuous Covariates |
Mean
(S.D.) |
Mean
(S.D.) |
F-Stat(p
value ) |
Mean
(S.D.) |
Mean
(S.D.) |
F-Stat(p
value ) |
Mean
(S.D.) |
Mean
(S.D.) |
F-Stat(p
value ) |
|
Husband Income |
24251.01
(13735.17) |
20825.397
(9741.07) |
3.76* |
24144.617
(13644.352) |
20428.571
(8968.19) |
2.54 |
24098.456
(13604.939) |
20896.552
(9685.574) |
1.58 |
|
Total Household income |
46402.423 (41013.55) |
41396.825 (11739.8) |
0.93 |
46309.987
(40316.587) |
39428.571
(12081.307) |
1.01 |
46235.521
(40179.49) |
40000
(12351.99) |
0.7 |
|
Per capita income |
2424.27 (1994.96) |
1819.199
(614.33) |
5.74* |
2403.952
(1964.452) |
1782.625
(625.703) |
3.48** |
2424.266
(1994.96) |
1819.199
(614.332) |
5.74** |
|
Poverty headcount |
0.84 (0.37) |
(0.968)
(0 .176) |
7.56 ** |
0.844
(0.363) |
0.971
(0.169) |
4.25** |
0.846
(0.362) |
0.966 (
0.186) |
3.16* |
|
Distance to Health Facility |
13.83
(10.81) |
12.94 (9.39) |
0.4 |
13.794
(10.754) |
(12.943)
9.698 |
0.21 |
13.748
(10.728) |
14
(10.278) |
0.02 |
|
Categorical Covariates |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
|
Residence: Rural/ Urban |
685(84.99) |
121(15.01) |
0.29 |
685
(84.99) |
121
(15.01) |
0.76 |
685
(84.99) |
121
(15.01) |
0.76 |
|
Type of House (Kacha/Pakka) |
377 (47) |
429
(53.23) |
1.38 |
429
(53.23) |
377
(46.77) |
1.36 |
429
(53.23) |
377
(46.77) |
0.35 |
|
Exposure to television |
516 (64) |
280( 36) |
3.84 |
516
(64.02) |
290
(35.98) |
0.91 |
516
(64.02) |
290
(35.98) |
1.28 |
|
Access to the health facility |
321(40) |
485(60) |
3.43* |
321
(39.83) |
485
(60.17) |
10.23*** |
321
(39.83) |
485
(60.17) |
4.43** |
|
Rooms for sleeping (<2/>=2) |
369 (46) |
437 (54) |
0.24 |
369
(45.78) |
437
(54.22) |
0.2 |
369
(45.78) |
437
(54.22) |
0.35 |
|
Access to Electricity |
765 (95) |
41(4.09) |
3.66 |
765
(94.91) |
41
(5.09) |
1.96 |
765
(94.91) |
103
(5.09) |
1.61 |
|
Perceived need factors |
|
|
|
|
|
|
|
|
|
|
Categorical Covariates |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
Number
(%) |
Number
(%) |
Chi
square (p value) |
|
beneficairy/ non- beneficiary |
408(50.62) |
398(49.38) |
65.73*** |
408
(50.62) |
398
(49.38) |
33.39*** |
398
(49.38) |
408
(50.62) |
26.78*** |
|
Place of residence: Rural/
Urban |
685(84.99) |
121(15.01) |
0.29 |
685
(84.99) |
121(15.01) |
0.13 |
685
(84.99) |
121
(15.01) |
0.76 |
|
Respondent employment status |
66
(8.56) |
737
(91.44) |
0.57 |
69
(8.56) |
737
(91.44) |
0.64 |
69
(8.56) |
737 (91.44) |
0.18 |
|
Joint or Nuclear Family System |
749
(92.93) |
57(7.07) |
5.20** |
749
(92.93) |
57
(7.07) |
2.78* |
749
(92.93) |
57
(7.07) |
2.29 |
|
HH arrangement (Owned/ Rented) |
644(79.9) |
162
(20.1) |
17.19*** |
644
(79.90) |
162
(20.10) |
9.20** |
644
(79.90) |
162
(20.10) |
7.57** |
|
Experience any Neonatal
Mortality |
503
(62.4) |
303 (38) |
0.81 |
503
(62.41) |
303(37.59) |
7.83** |
503
(62.41) |
303
(37.59) |
2.56* |
|
Complications in past delivery |
616
(76.5) |
189
(23.48) |
1.38 |
616
(76.52) |
189
(23.48) |
1.72 |
616
(76.52) |
189
(23.48) |
0.65 |
|
Birth Interval |
657(82) |
149 (19) |
8.54** |
657
(81.51) |
149
(18.49) |
2.39 |
657
(81.51) |
149
(18.49) |
2.68* |
|
Vaccinated during ANC |
610 (76) |
196 (24) |
2.87 |
610
(75.68) |
196
(24.32) |
3.69 |
610
(75.68) |
196
(24.32) |
3.45 |
|
Tetanus toxoide vaccination |
560 (70) |
246 (30) |
0.05 |
246 (30.52) |
560(69.48) |
1.01 |
246
(30.52) |
560
(69.48) |
0.58 |
The income per
capita serves as an indicator of the community’s overall social and economic
well-being. Per capita income is linked to medical facilities, transportation,
health, education and MHC awareness. This study calculates per capita income
using household size. Higher per capita income assists individuals in managing
CoC costs. Both spouse income and per capita income are associated with SBA's
utilisation of ANC services, followed by PNC. Families with higher income and
per capita income used MHC services more. Participants who received financial
assistance (like the CCT) increased the likelihood of receiving ANC from the
SBA. Access to health facility significantly
associated with MHC service utilisation. If getting to a hospital is difficult,
MHC service utilisation will reduce. The location of one's home also has a
positive and significant effect on the utilisation of preventative
MHC services. MHC services are more popular in urban than rural areas.
Respondents who own a home are more likely to receive MHC than a renter.
Multivariate
logistic regression examined ANC, PNC, and SBA utilisation. Predisposing,
enabling, and perceived need variables affect health care seeking.
Among predisposing factors age of a woman at first delivery,
their education, household size, and health care provider all affect CoC
use. Table 3 lists predisposing, enabling, and perceived need factors for MHC
during delivery. The model I examines ANC correlations. This study found a
statistically significant connection between women's age at first birth,
respondent and spouse's education level with ANC usage from SBA as educated
partners tend to have higher use of ANC service from a skilled provider, where
it decreases with larger household size.
Table 3. Multinomial Logistic Regression of Predisposing, Enabling and Perceived Factors of Women of K.P., who had Received ANC, SBA and PNC
|
ANC |
Care
at Delivery assisted by SBA |
PNC
followed with ANC and Delivery |
||||||||||
|
|
followed
with ANC |
assisted
by SBA |
||||||||||
|
Variables
|
Logit
model |
Probit
Model |
Logit
model |
Probit
Model |
Logit
model |
Probit
Model |
||||||
|
|
Coefficients
(S.E.) |
P
value |
Coefficients
(S.E.) |
P
value |
Coefficients
(S.E.) |
P
value |
Coefficients
(S.E.) |
P
value |
Coefficients
(S.E.) |
P
value |
Coefficients
(S.E.) |
P
value |
|
Predisposing
factors |
|
|
||||||||||
|
Age |
-.0321
(0.027) |
0.247 |
-.0177
(0.0152) |
0.245 |
-0.0308
(0.0527) |
0.559 |
-0.0160
(0.027) |
0.556 |
-.00651
(0.0529) |
0.902 |
-0.0056 (0.028) |
0.839 |
|
Age at first birth |
0.1377*
(0.065) |
0.035 |
0.0723*(0.0346) |
0.037 |
-0.00094
(0.094) |
0.992 |
-0.0064
(0.048) |
0.893 |
-.0401
(0.0955) |
0.674 |
-0.027
(0.049) |
0.578 |
|
Women total years
of schooling completed |
.0943*
(0.0447) |
0.035 |
0
.048* (0.0244) |
0.052 |
0.0793
(0.0680) |
0.243 |
0.0246
(0.036) |
0.498 |
0.123
(0.0685) |
0 |
0.0504
(0.036) |
0.067 |
|
Husband years of
schooling |
.1134* (0
.065) |
0.082 |
0.0614*
(0.0351) |
0.08 |
-0.0356
(0.1029) |
0.729 |
-0.0167
(0.054) |
0.76 |
-0.0886
(0.1015) |
0.382 |
-0.046
(0 .0548) |
0.403 |
|
Total Household
size |
-.0389*
(0.0210) |
0.064 |
-0.000276 |
0.047 |
-0.0221
(0.033) |
0.5 |
-0.0097
(0.0177) |
0.582 |
-.0114
(0.0320) |
0.721 |
-0.0045
(0.0175) |
0.797 |
|
Live pregnancies |
-.1244
(0.2218) |
0.575 |
-.0263
(0.1157) |
0.82 |
-0.764
(0.4176) |
0.067 |
-0.3415
(0.2119) |
0.107 |
-0.553
(0.4007) |
0.169 |
-0.238
(0.2064) |
0.249 |
|
Total number of
pregnancies |
-.0087
(0.195) |
0.964 |
-0.0329
(0.1034) |
0.75 |
0.4176
(0.358) |
0.244 |
0.1952
(0.1864) |
0.295 |
0.1763
(0.3423) |
0.607 |
0.078 (0
.1810) |
0.665 |
|
Health services
provider (Skilled/ Unskilled) |
2.748* (0
.3832) |
0 |
1.552
(0.2127) |
0 |
6.236
(1.1257) |
0 |
2.891
(0.4124) |
0 |
5.716
(1.01) |
0 |
2.623
(0.4088) |
0 |
|
Enabling factors |
||||||||||||
|
Residence: Rural/
Urban |
-1.592
(0.5126) |
0.002 |
-0.855
(0.269) |
0.001 |
-1.381
(0.7099) |
0.052 |
-0.8172
(0.403) |
0.042 |
-.9989
(0.677) |
0.14 |
-0.6063
(0.385) |
0.115 |
|
Exposure to
television |
.0396
(0.2513) |
0.875 |
0.0420
(0.1354) |
0.756 |
0.5212
(0.4291) |
0.224 |
0.089
(0.209) |
0.669 |
0.393
(0.417) |
0.346 |
0.0482
(0.2072) |
0.816 |
|
Access to health
facility |
07712
(0.2224) |
0.729 |
0.042
(0.1165) |
0.722 |
1.043
(0.413) |
0.012 |
0.4443
(0.207) |
0.032 |
0.6719
(0.403) |
0.095 |
0.2738
(0.2042) |
0.18 |
|
Perceived need
factors |
||||||||||||
|
Status |
5.0329
(1.060) |
0 |
2.416
(0.4247) |
0 |
4.744
(1.154) |
0 |
2.383
(0.506) |
0 |
4.38
(1.152) |
0 |
2.161
(0.5012) |
0 |
|
Birth Interval (<1/>=2
years) |
-2.009
(0.675) |
0.003 |
-1.184
(0.379) |
0.002 |
-1.254
(0.7727) |
0.105 |
-0.8178
(0.4344) |
0.06 |
-1.645
(0.8801) |
0.062 |
-0.9834
(0.479) |
0.04 |
|
Have you been
vaccinated during ANC |
-.0611
(0.4162) |
0.883 |
-0.000
(0.2242) |
1 |
0.936
(0.7630) |
0.22 |
0.560
(0.416) |
0.179 |
1.146 (0.7867) |
0.145 |
0.644
(0.4353) |
0.139 |
|
TFR Vaccination |
-.3407
(0.4215) |
0.419 |
-.1292
(0.2260) |
0.568 |
-0.335
(0.7303) |
0.647 |
-0.284
(0.385) |
0.461 |
-0.0648
(0.7001) |
0.926 |
-0.1344
(0.3772) |
0.722 |
|
Number of obs |
806 |
806 |
806 |
806 |
806 |
806 |
||||||
|
LR chi-square (p
value) |
175.32 |
175.29 |
0 |
185.6
(0.00) |
181.59
(0.00) |
145.62
(0.00) |
142.44
(0.00) |
|||||
|
Log likelihood |
-133.39356 |
-133.40956 |
-51.26 |
-53.218434 |
-52.081159 |
-53.66948 |
||||||
|
Pseudo R2 |
0.4 |
0.3965 |
0.6444 |
0.6305 |
0.583 |
0.5703 |
||||||
The variable SBA was positively related to
CoC (ANC to SBA) and PNC. This suggests that women are more likely to use MHC
services if the health care provider is skilled in this regard. Women in rural
areas are less likely to seek ANC care because they lack access to modern
health care facilities. According to previous research, urban mothers are more
likely to seek out medical attention (Tesema et al., 2002;
Nigussie
et al., 2004;
WHO,
2003), as
these women have better access to health care, public relations and formal
education.
Among the perceived need factors, status and birth
interval are associated with ANC use. The study found that respondents who got
economic assistance were more likely to receive ANC from SBA.
The study indicated that respondents with a birth interval of less than a year
are less likely to use skilled ANC. This is because the more children a woman
has, the more expensive it is for her to receive ANC treatments from an
institution due to the user fee and transportation costs. Model
II examines the correlations between ANC and SBA utilisation. All significant
variables remained in the second model except for women's and spouses'
education. Additionally, we discovered a substantial correlation between live
births and access to health care for model II.
Model III examines CoC from ANC to birth and postpartum in women who got MHC services from skilled attendants. Model III had all of Model II's qualities, and model III stresses more mothers' education in acquiring PNC. Perhaps this is due to the fact that educated women have better access to contemporary health care and are more likely to utilise MHC services.
Discussion of Results
While focusing particularly on maternity and newborn health outcomes, the government of K.P. should priorities CoC as a primary strategy. It advocates for an integrated health care system that connects all levels of ANC, SBA, and PNC. However, because the data on CoC is inadequate, we cannot accurately analyse the province's position in terms of CoC. As such, this study will examine the factors that impede the CoC from delivery to the postpartum period.
According to studies, complications during childbirth and postpartum increase maternal mortality (Bustreo et al., 2013). Around a quarter of pregnant women in K.P. don't receive prenatal care, and half don't deliver in a hospital. (Bhutta et al., 2013; Bustreo et al., 2013; WHO, 2014). The majority of deliveries still occur at home in K.P. (NIPS, 2013). In comparison to other provinces of Pakistan, the rate of receiving ANC services is quite low in K.P. In Kohistan or Tor Ghar, ANC visits averaged 361 and 199 in the first quarter of 2018. However, this study showed a substantial increase in the rate of CoC completion. The main reason attributed could be the awareness that an expecting mother has during exposure to the MHC care program, i.e. Chief Minister initiative for pregnant women in K.P. (CCT program2014), their childbearing age, level of education, and kind of health service provider.
Nonetheless, women in K.P. continue to experience a lack of continuity of treatment at all three levels. Most dropouts occur between ANC and SBA delivery, probably due to limited ANC and home-based deliveries. In K.P., lack of access to a health facility drives home births. This is due to structural and cultural limits in Pashtoon society, as well as traditional orthodox traditions like TBA (Sarfraz & Hamid, 2014; Iqbal, 2017), as more than half of residential deliveries are made without SBA help (Sarfaraz & Hamid, 2014).
With the exception of ANC visits, women who live more than an hour from a health care institution are eight times more likely to deliver at home than those who do not. Similarly, women who have had SBA during delivery are more likely to obtain PNC (Iqbal et al., 2017; Wang & Hong, 2015). Most women are abandoned following ANC and do not receive appropriate delivery support or PNC for themselves or their newborns. Our results show that strengthened CoC requires health facilities and experienced healthcare professionals. High-quality ANC helps women understand pregnancy complications and the need for SBA. Most mothers who received appropriate birth assistance and PNC for the first 48 hours improved MCH significantly. Our analysis shows that most reproductive stage determinants, such as older age at first birth, higher level of education, fewer children, and spouse's level of education, are directly correlated with CoC components (ANC, SBA, and PNC) utilisation in K.P. when combined with enabling factors such as rural or urban residence and access to health facilities.
Women with less than a year birth interval, larger families, and more than two children are less likely to receive these services. Given the study's descriptive nature, this could be coincidental. Previous studies in Ghana, Tanzania, India, China, and Cambodia verify these findings (Gao et al., 2010; Ghazi et al., 2012; Rishworth, 2014; Wang & Hong, 2015; Yejj et al., 2015 ).
The study found respondents' education level as a significant predictor of CoC as women with a higher level of education are more expected to use MHC services (Olanyinka et al., 2014; Iqbal et al., 2017; Dahiru & Oche, 2015; Ononokpono & Odimegwu, 2014; Singh & Jha, 2016). Unfortunately, women's education levels are significantly lower, as the study reports respondents have an average of six years of schooling. Approximately 85 per cent of sample respondents are from rural areas. Thus, rural women confront health care access issues due to topography, roads, and public transit (Karkee et al., 2013; Olanyinka et al., 2014). Similarly, fewer K.P. women get continuous care. At the same time, total live births and birth interval affected CoC negatively.
Women who have more than one child with a birth gap of less than a year are less likely to use MHC throughout pregnancy and postpartum (Iqbal et al., 2017; Olayinka, 2014; Terekegan et al., 2014). The study's findings highlight the relevance of community-based health care programs supporting MHC continuity, which may reduce MCH accessibility barriers. Home visits and outreach programs could help rural and impoverished women get ANC and PNC services (Jennings et al., 2017). The availability of modern MHC treatments is linked to service utilisation, which affects treatment-seeking behaviour and pregnancy outcomes (Singh et al., 2012; Ray et al., 2018; Zakar, 2017).
In K.P., education, age, spouse education, the total number of children, health care provider, residence location, and availability to health facility indicate ongoing MHC utilisation from pregnancy to postpartum. Thus, discontinuation of CoC use in K.P. is associated with typical structural and cultural constraints in Pashtun society, including the traditional orthodoxy's function of DAI (Sarfraz & Hamid, 2014), restrictions on women's spatial mobility (ADB, 2000), and women's family autonomy (Ghazi, 2012).
Iqbal et al. (2017) studied CoC in Pakistan; however, no such study has been done in K.P. This work also contributes to existing knowledge in the following ways. Unlike other surveys, this study used a structured questionnaire on 806 respondents from five randomly selected areas (namely Peshawar, Swabi, Nowshera, Malakand and Kohat). Second, most surveys can't follow ANC or PNC visits. This study calculates ANC and PNC services assisted by SBA based on patient visits. This helps us understand the reasons for care discontinuity and proposes ways to reduce it.
The study has other drawbacks, though. Cross-sectional surveys can't show causal linkages. Second, many district union councils were inaccessible owing to the pandemic Covid-19 because most people dislike face-to-face interviews. Thus, self-reports may influence the survey's results. Owing to the sample's representativeness for each district and a response rate of 98 per cent, this does not alter the generalizability of the findings.
Conclusion
KP has fewer ANC visits followed by SBA and PNC delivery than other provinces. Despite a minor rise in ANC visits, CoC progress is unsatisfactory. This study examines factors that affect CoC from pregnancy through postpartum. The study indicates substantial dropout during delivery and postpartum. The factors associated include household size, the total number of live pregnancies, place of residence, and shorter birth intervals. At the same time, education of women, age at first birth, health facility access, and cash transfers improve the likelihood of getting ANC, SBA, and PNC.
There is limited literature available in exploring the determinants of MHC service utilisation and correlates of CoC in Pakistan (Iqbal, 2017; Sarfraz & Hamid, 2014, Zakar et al.,2017), but a huge deficiency exists in explaining the main factors responsible for low utilisation of CoC services in K.P. K.P.'s maternal program aims to improve MNCH quality and continuity. It provided free birth care and cash incentives to women who had at least four prenatal sessions. Also, free neonatal care is offered (Govt of KPK, 2014). High dropout rates during SBA-assisted birth indicate addressing supply-side restrictions, such as drug and health professional shortages. The study further suggests addressing supply-side barriers to better assist the expecting mother during and after delivery (Austin et al., 2011; Jacob et al., 2011).
Other suggested strategies should include media campaigns, health education workshops, specialised workers, and community-based initiatives. SBA, community-based interventions, and women's education boost ANC coverage and institutional delivery Ray, 2018; Mbuagbaw et al., 2015). K.P. women should be included in designing these initiatives, which should be targeted to their specific needs. Both the public and private sectors should be engaged in building health systems that eliminate CoC obstacles.
References
- Akinyemi, J. O., Afolabi, R. F., & Awolude, O. A. (2016). Patterns and Determinants of Dropout from Maternity Care Continuum in Nigeria. BMC Pregnancy Childbirth. 16(1), 282
- Anderson, R. M. (1995). Revisiting the behavioral model and access to medical care: does it matter? Andersen RM J Health Soc Behav. Mar; 36(1), 1-10.
- Andersen, R., & Newman, J. F. (2005). Societal and Individual Determinants of Medical Care Utilisation in the United States. Milbank Q. 2005, 83(4), 1-28.
- Annual reports. (2014). Department of Maternal New Born Child Health Services. Annual Report 2014-15. Peshawar, Pakistan: Government of Pakistan, Ministry of Health and Population.
- Austin, A., Langer, A., Salam, R. A., Lassi, Z. S., Das, J. K., & Bhutta, Z. A., (2014). Approaches to improve the quality of maternal and newborn health care: an overview of the evidence. Reproductive Health, 11(2), S1.
- Baral, Y., L., Skinner, J., & Teijlingen, E. (2010). Determinants of Skilled Birth attendants for delivery in Nepal. KUMJ, 8(31), 325– 332.
- Berhan, Y., & Berhan, A. (2014). Antenatal care as a means of Increasing Birth in the Health Facility and Reducing Maternal Mortality: A systematic review. Ethiop J Health Sci, 24, 93–104.
- Bhutta, Z. A., Das, J. K., Bahl. R., Lawn, J. E., Salam, R. A., & Paul. V. K., et al. (2014). Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? The Lancet. 384(9940), 347–370.
- Bustreo, F., Say, L., Koblinsky, M., Pullam, W. T., Temmerman, M., & Pablos, M. (2013). Ending preventable maternal deaths: the time is now. The Lancet Global Health 1:e176–e177.
- Campbell, O. M., & Graham, W. J. (2006). Strategies for Reducing Maternal Mortality: Getting on With What Works. The Lancet 2006, 368(9543), 1284–1299.
- Chakaraborty, M. et al., (2003). Determinants of the use of maternal health services in rural Bangladesh NITAI Health Promotion International. 18(4), Oxford University Press. doi: 10.1093/heapro/dag414
- Chandrashekar, S., Rao, R. P., Nair, N. S., & Kutty, P. R. (1998). Socio-Demographic determinants of Antenatal Care. Tropical Doctor, 28(4), 206-9.
- Cropper, M. L. (1977). Health, Investment in Health, and Occupational Choice. Journal of Political Economy. 85(6), 1273–94.
- Dahiru, T., & Oche, O. M. (2015). Determinants of antenatal care, institutional delivery and postnatal care services utilisation in Nigeria. Pan Afri Medl J, 22(1),
- Darmstadt, G. L., Bhutta, Z. A., Cousens, S., Adam, T., Walker, N., & Bernis, L., et al. (2005). Evidence-based, Cost effective Interventions: How many Newborn Babies can we save? The Lancet, 365(9463), 977–988.
- De Graft, J. et al. (2006). The Maternal Newborn and Child health: Continum of Care. World Health Organisation.
- DHIS. (2018). Demographic Health Information System. Health Survey 2017- 18. Islamabad, Pakistan, National Institute of Population Studies and Macro International Inc; National Institute of Population Studies (NIPS) and Macro International. In: Inc
- Dixit, P., Dwivedi, L. K., & Ram, F. (2005). Estimating the Impact of Antenatal care Visits on Institutional Delivery in India: A Propensity score matching analysis. Health. 5(05), 862-78.
- Dwivedi, L. K., & Reshmi, R. S. (2009). Role of antenatal care in utilising maternal health care services in Maharashtra. In: Singh, K. K., Yadava, R, C., Pandey, A., eds. Population, Poverty and Health. New Delhi, Hindustan Publishing Corporation. 207-16.
- Gao, Y., Barclay, L., Kildea, S., Hao, M., & Belton, S., (2010). Barriers to increasing hospital birth Rates in rural ShanxProvince, China. Reprod Health Matters. 18, 35–45.
- Ghazi, T. M., Moudi, Z., & Vedadhir, A. (2012). Home birth and barriers to referring women with obstetric complications to hospitals: A mixed methods study in Zahedan, Southeastern Iran. Reprod Health. 9(5), 29.
- Govindasamy, P., & Ramesh, B. M. (1997). Maternal Education and the Utilisation of Maternal and Child Health Services in India. Mumbai, International Institute for Population Sciences and Calverton, Maryland, Macro International Inc; 1997.
- Iqbal, S., Maqsood, S., Zakar, R., Zakar, M. Z., & Fischer, F. (2012).Continuum of Care in Maternal, Newborn and Child health in Pakistan: Analysis of trends and determinants from 2006 to 2012. BMC Health Services,17(1), 189.
- Jacobs, B., Bigdeli, M., Annear. P. L., & Van, W. D. (2011) Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy. Plan 2011, 27(4), 288–300.
- Jennings, M. C., Pradhan, S., Schleiff, M., Sacks, E., Freeman, P. A., & Gupta, S., et al. (2017). Comprehensive review of the evidence regarding the effectiveness of community–based primary health care in improving maternal, neonatal and child health: 2. maternal health findings. Journal of Global Health, 7(1),
- Joshi, C., Torvaldsen, S., Hodgson, R., Hayen, A., Factors Associated with the use and Quality Of Antenatal care in Nepal: A population-based study using the demographic and health survey data. BMC Pregnancy Childbirth, 14(1):94.
- Katahoire, A., Scheutz, F., Sabore, S., & Whyte, S. R. (2004). The importance of maternal schooling for child morbidity and mortality and maternal health behavior in southern Uganda. Journal of Health & Population in developingcountries (/
- Karkee, R., Lee, A. H., & Binns, C. W. (2013). Birth Preparedness and Skilled Attendance at birth in Nepal: Implications for achieving millennium development goal 5, 29(10), 1206–1210.
- Kerber, K. J., de Graft, J. E., Bhutta, Z. A., Okong, P., Starrs, A., & Lawn, J. E. (2007). Continuum of Care for Maternal, newborn, and child health: From slogan to Service Delivery. The Lancet, 370(9595), 1358–1369.
- Khanal, V., Adhikari, M., Karkee, R., & Gavidia, T. (2014). Factors Associated with the Utilisation of postnatal Care Services among the Mothers of Nepal: Analysis of Nepal demographic and health survey 2011. BMC Womens Health 2014, 14(1), 19.
- Khan, M. et al., (2006). Geographic aspects of poverty and health in Tanzania: does living in a poor area matter? Hutchinson PL Health Policy Plan. Mar; 21(2), 110-22.
- Mbuagbaw, L., Medley, N., Darzi, A., Richardson, M., Habiba, G. K., & Ongolo- Zogo, P. (2015). Health system and community level interventions for improving antenatal care coverage and health outcomes. Cochrane. Database Syst Rev 2015, 12(12),
- Nigussie, M., Haile, Mariam, D., & Mitike, G. (2004). Assessment of safe delivery service Utilisation among women of child bearing age in North Gondar Zone, Northwest Ethiopia. Ethiop J Health Dev. 18(3), 145-152.
- Olayinka, O. A., Achi, O. T., Amos, A. O., & Chiedu, E. M. (2014). Awareness and barriers to utilisation of maternal health care services among reproductive women in Amassoma community, Bayelsa State. Int J Nurs Midwifery, 6(1), 10–15.
- Ononokpono, D. N., & Odimegwu, C. O. (2014). Determinants of maternal health care utilisation in Nigeria: a multilevel approach. Pan Afr Med, 17(Suppl 1)
- Ray, S. et al., (2018). Utilisation pattern and associated factors of maternal health care services in Haryana, India: a study based on district level household survey data, International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 7(3), 1154-1163.
- Rishworth, A. C. (2014). Women’s Navigation of Maternal Health Services in Ghana’s Upper West Region in the Context of the National Health Insurance Scheme.
- Rockers, P. C., Wilson, M. L., Mbaruku, G., & Kruk, M. E. (2009). Source of Antenatal care Influences Facility delivery in rural Tanzania: A Population-based study. Maternal Child Health. 13(6), 879.
- Sarfraz, M., & Hamid, S. (2014). Challenges in delivery of skilled maternal care: Experiences of community midwives in Pakistan. BMC Pregnancy Childbirth, 14(59),
- Shrestha, S. K., Banu, B., Khanom. K., Ali. L., Thapa, N., & Stray-Pedersen, B., et al. (2012). Changing trends on the place of delivery: why do Nepali women give birth at home? Reproductive Health, 9(1), 25.
- Singh. D. R., & Jha, T. (2016). Exploring Factors Influencing Antenatal Care Visit Dropout at Government Health Facilities of Dhanusha District, Nepal. Am J Public Health, 4(5), 170–175.
- Singh, P. K., Rai, R. K., Alagarajan, M., & Singh, L. (2012). Determinants of maternity care services utilisation among married adolescents in rural India. PloS one. 7(2), 31666.
- Tarekegn, S. M., Lieberman, L. S., & Giedraitis, V. (2014). Determinants of maternal health service utilisation in Ethiopia: Analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth, 14(1), 161.
- Tesema, F., Assefa. M., & Ayele, F. (2002). Mothers' health services utilisation and health care seeking behavior during infant rearing: A longitudinal community-based study, South West Ethiopia. Ethiop J Health Dev, 16 (Special Issue), 51-58.
- Thadeus, & Maine M. (1994). Too far to walk: Maternal mortality in context. Soc Sci Med. 1994, 38 (8), 1109-1120.
- Thind, A., Mohani, A., Banerjee, K., & Hagigi, F. (2008). Where to deliver? Analysis of choice of delivery Location from a National Survey in India. BMC Public Health. 8(1), 29.
- Wagle, R. R., Sabroe. S., & Nielsen, B. B. (2004). Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth, 4(1), 8.
- Wang, W., & Hong, R. (2015). Levels and determinants of continuum of care for maternal and Newborn health in Cambodia-evidence from a population- based survey. BMC Pregnancy Childbirth, 15(1),62.
- WHO. (2012).? Trends in maternal mortality: 1990 to 2010. WHO, UNICEF, UNFPA and The World Bank estimates? In. Geneva. 236
- WHO. (2018).? World Health Statistics. In: WHO Library Cataloguing-in-Publication Data. Geneva: World Health Organisation.
- WHO, UNICEF, UNFPA, NIPS and World Bank. (2007). Maternal Mortality in 2005, Geneva: WHO Press [Online]? Available on WHO
- WHO. (2012, 2013). Trends in maternal mortality: 1990 to 2010. WHO, UNICEF, UNFPA and The World Bank estimates. In. Geneva. 236
- WHO. (2003, 2005). World Health Organization. Antenatal care in developing countries: promises, Achievements and missed opportunities: an analysis of trends, levels and differentials 1990-2010. (Various Reports) Geneva: WHO; 2003. 17.
- Yeji, F., Shibanuma. A., Oduro, A., Debpuur, C., Kikuchi, K., & Owusu, S., et al. (2015). Continuum of care in a maternal, newborn and child health program in Ghana: Low completion rate and multiple obstacle factors. PloS One. 10(12), e0142849.
- Zakar, R., et al., (2017). Determinants of maternal health care services utilisation in Pakistan: evidence from Pakistan Demographic and health survey, 2012-13, Journal of obstetrics and gynaecology, 37(3), 330-337.
Cite this article
-
APA : Majeed, R., Iqbal, J., & Haq, Z. u. (2022). Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan. Global Economics Review, VII(II), 68-89. https://doi.org/10.31703/ger.2022(VII-II).07
-
CHICAGO : Majeed, Rabia, Javed Iqbal, and Zahoor ul Haq. 2022. "Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan." Global Economics Review, VII (II): 68-89 doi: 10.31703/ger.2022(VII-II).07
-
HARVARD : MAJEED, R., IQBAL, J. & HAQ, Z. U. 2022. Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan. Global Economics Review, VII, 68-89.
-
MHRA : Majeed, Rabia, Javed Iqbal, and Zahoor ul Haq. 2022. "Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan." Global Economics Review, VII: 68-89
-
MLA : Majeed, Rabia, Javed Iqbal, and Zahoor ul Haq. "Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan." Global Economics Review, VII.II (2022): 68-89 Print.
-
OXFORD : Majeed, Rabia, Iqbal, Javed, and Haq, Zahoor ul (2022), "Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan", Global Economics Review, VII (II), 68-89
-
TURABIAN : Majeed, Rabia, Javed Iqbal, and Zahoor ul Haq. "Determinants of Continuum of Care: Evidence from the Conditional Cash Transfer Program of the Khyber Pakhtunkhwa Pakistan." Global Economics Review VII, no. II (2022): 68-89. https://doi.org/10.31703/ger.2022(VII-II).07
